Our articles are not designed to replace medical advice. If you have an injury we recommend seeing a qualified health professional. To book an appointment with Tom Goom (AKA ‘The Running Physio’) visit our clinic page. We offer both in-person assessments and online consultations.
Running isn’t the only thing that can cause an injury. It might seem obvious but it’s something many runners and some clinicians seem to forget. Identify other causes and you’ll reduce injury risk, recover quicker and run more…
I had a flare-up of some old niggles last week. My left knee was stiff and sore, my right Achilles was tender and making a clicking noise when I moved. I felt like I was recovering from an epic run, but sadly I wasn’t – I hadn’t run in nearly 2 weeks. What caused my pain was moving home and renovating our new place. All the crouching, lifting, carrying and kneeling took its toll. I wasn’t troubled by a 20-mile trail race up some of the biggest hills I’ve ever seen but I have been defeated by a 2-bed bungalow!
How can you tell if running is causing your symptoms?
In some situations it’s really clear that running is the culprit – you run, it hurts, you don’t run, it doesn’t. Simples. But in many injuries, it isn’t that clear especially if the pain doesn’t occur during activity and comes on after. Many conditions actually improve with movement and worsen with inactivity and this can confuse things too. The classic example is low back pain – many people find that they can run, swim, go to the gym etc but if they sit for too long they’re in pain.
If you aren’t sure what is aggravating your pain try making a pain diary. Make a brief note of what you’ve done during the day and what your pain levels are (e.g. scoring it out of 10 where 0 is no pain and 10 is the worst pain you can imagine). Remember to record periods of inactivity too and that it can take 24-48 hours for things to be sore after some activities. This can be really useful in identifying patterns with your symptoms and give you indications on what to modify. When I had ITBS in the past I discovered that the key factor for me was running speed – I could manage long slow runs pain-free but even short speed sessions aggravated my symptoms. I reduced my speed work for a couple of weeks and things improved significantly. I’ve gradually reintroduced it and can now do 10-mile tempo runs at sub 7-minute mileage with no problems.
If you can identify what aggravates your symptoms and change these activities you’ll have less pain and be able to run more. Win-win!
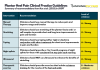
Common aggravating factors
Patellofemoral Pain Syndrome – Squatting, up/down stairs, kneeling, prolonged sitting, walking downhill
ITBS – cycling, gym work – leg press, leg extension, deep squats, hill walking. Any activities that involve repeatedly flexing the knee beyond 30-40 degrees.
Achilles tendinopathy – walking (especially up hills), repeated squatting, up/downstairs
Plantar Fasciitis – walking (especially barefoot), prolonged standing, squatting
Back pain – very variable depending on the cause but back pain can be aggravated by prolonged sitting, standing or lying, walking, driving, lifting, carrying, bending, coughing and sneezing (and a host of others).
Reducing aggravation – pacing and modification
Decreasing the impact of aggravating factors doesn’t have to be done simply by avoiding them altogether. For example, if cycling aggravates your ITBS you needn’t stop totally but change it to a level that doesn’t increase your pain. Total avoidance of an activity is rarely the answer. It might be useful as a short term measure if you are in severe pain or recovering from an acute injury but it’s not a good long term strategy.
Pacing is often a better solution than total avoidance. Pacing means doing things in small manageable amounts rather than overdoing it or pushing on through pain. If I had paced myself when renovating our new home rather than spending 6 hours squatting and kneeling to replace our flooring I probably wouldn’t have a sore knee!
Part of pacing is modifying activity to make it easier and less likely to provoke pain. Some years ago I treated a delightful lady who had 7 children at home. She said her days were spent doing round after round of washing. She’d place her washing basket on the floor outside and bend to pick up each item to put it on the washing line. The repeated bending and lifting was giving her severe back pain but simply stopping doing the washing wasn’t an option. She found a solution that did more for her pain than any other treatment – she found an old chair with wheels on and put the washing basket on that. Instead of bending to the floor again and again she’d just pick the clothes from the basket on the chair, and then move it to the next section of the washing line. A simple but very effective bit of modification made a huge difference for her.
Some modifications might help an injury you’re struggling with. If cycling aggravates your ITBS try raising your seat a little, if kneeling hurts your knee put a cushion on the floor or use a gel pad. If driving hurts your back try moving the seat a little or placing a rolled-up towel in your lower back.
See the bigger picture
When managing an injury it is easy to get drawn into what is happening now, right at this moment, sometimes though you need to see the bigger picture – what’s happened in the last week and the last month? Take, for example, a patient I saw recently who had calf pain after a 30-minute run. “I don’t understand,” she said, “I’ve run for an hour without calf pain and yet this hurt after 30 minutes, what’s going on?”. When we looked back through the week we found the answer – in the days leading up to the run she’d run a 10k and done strength work on the calf – the muscle was fatigued before she’d even started the run! Here the cause isn’t the running so much as the lack of rest and recovery between each activity. The point to take from this is to plan your schedule carefully and give your body time to recover, adapt and strengthen in response to exercise.
Do I continue to run if injured?
According to a Runner’s World survey around 66% of runners carry an injury, if all runners stopped when injured there would be hardly anyone left running! That doesn’t mean though that it is always best just to carry on regardless and clearly with traumatic injuries like fractures or severe sprains you wouldn’t be able to run! (The plaster cast really messes up your running form!)
When recovering from injury be guided by your health professional on whether to run and how much to do.
That said this can be a contentious issue. Without meaning to criticise fellow clinicians there are some unusual decisions made in managing runners. I’ve seen many told not to run even a year after fairly minor injuries. Try and have a detailed discussion with your health professional – if they are telling you not to run ask why and try to agree on a time frame on returning to running. If you have been running a little when managing an injury with no problems tell them this. With good communication with your health professional, you may find they’ll be happier for you to continue your running. Wherever possible I try to modify things to keep people running. This might be a change of running surface, reducing distance, speed, intensity etc. Even then there are times when I will suggest that a runner hangs up their shoes for a little while. Especially if symptoms just aren’t settling despite rehab and modifying training.
As a very general rule if you have no history of trauma, no swelling, joint locking or giving way and you can find a way to run with no pain then you can continue to run. What it comes down to though is a judgement call on the part of the runner, more here on whether to run or not and remember if in doubt get it checked out!
Closing thoughts: sadly running is still looked upon in some areas as a sport that ‘wears out your joints’ and the first line of treatment of any injury is to stop. This needn’t be the case and with a little thought around what else might be causing your pain and how you can modify these activities your symptoms will improve and in many cases, you’ll be able to keep running.